If you do private consultations in forensic pathology, you will occasionally be asked to write a report for presentation to the opposing counsel. There are basically two kinds of reports we as FPs put out: Autopsy reports and consultation reports. This is about the latter. As a private consultant, I *hate* doing second autopsies, so I’m not going to talk about writing them — I do them just like a regular autopsy report, and if you are reading this you should know how to do that.
The kind of consultation report I am talking about is one where you are given a case. You might get an autopsy report (in a wrongful death case), medical records, previous deposition transcripts, videos of interviews, police reports, bodycam footage, whatever. One of the interesting things about doing these cases is that as a private consultant I get a *lot* more information than I get when I do a regular autopsy in my jurisdiction. Go figure. So, you sit down, go through all of these, and come to some conclusion. Generally, if you are writing a report, that means that your conclusions are different than those of the expert on the opposing side. Sometimes you write an initial report, then there are depositions, then you get the opposing experts report. Then you’ll write a second report as a rebuttal to the points the opposing expert makes.
So, I thought I’d write a little about how I write a report, and some of the things I’ve seen on other people’s reports.
When I write a report, it usually has a very structured format:
- A review of my qualifications
- A list of the materials I’ve reviewed
- My mandate (I’ll talk about this later)
- An executive summary succinctly addressing the mandate
- A point by point explanation of my findings
- A summary
- References
Note that there’s something missing in my reports that is found in many others — A review of the facts of the case. If counsel insists, I will put it between 2 and 3. I don’t like to do a review of the case because in my experience many of the things that happened are not relevant to my testimony, but I have to mention them if I’m going to give a timeline or whatever. In that case, at deposition or at trial, opposing counsel will pimp me on details of that timeline that I just don’t think are relevant and I’m just taking on faith anyway, e.g.
“Doctor, you state in your report that the decedent cried out ‘Stop, stop, you fiend!” How do you know that? What is your basis for making that claim?”
“Er, counsel told me.”
“So, as far as you know, this part of your report is false.”
“Doh. I guess.”
I hate it when that happens.
Nonetheless, sometimes counsel will insist, and I’ll do it. It means I have to try to remember exactly where in the five million pages of stuff I’ve gone through I picked out that little gem…
Now on to the stuff I feel is important.
Please note in the following that I’m providing massaged pieces of different cases, so the “report” here will not flow — each part is from a different consult modified to be anonymized.
- Review of qualifications.
The review of qualifications need not be long, but I always include my education, board certifications, licensure, and generally the stuff that will be in your voir dire when you are on the stand. Some clients want this short, some want it long. Some want me to emphasize cases of national interest i’ve worked on, some want me to avoid it. Here’s my standard “qualifications” section:
I received my MD from Vanderbilt University School of Medicine. I then completed my residency in Anatomic and Clinical Pathology, graduate school in Computer Science, and fellowship in Forensic Pathology at the University of North Carolina at Chapel Hill. Following my training in North Carolina, I joined the U.S. Army and was stationed at the Armed Forces Institute of Pathology as Staff Pathologist in Molecular Pathology, Director of the Scientific Computing Laboratory, and Deputy Medical Examiner for the Office of the Armed Forces Medical Examiner.
Following my military service, I was recruited by the Georgia Bureau of Investigation as Northwest Regional Medical Examiner, where I also received my Master’s Degree in Justice Administration.
I then accepted the position as Professor of Pathology and Director of Autopsy and Forensic Services at Brody School of Medicine at East Carolina University in Greenville, NC.
Following my retirement from East Carolina, I worked as Assistant Medical Examiner for Knox and Anderson Counties in Knoxville TN until my second retirement in 2021. I continue to serve as an Assistant Medical Examiner for Knox County and perform investigations part time as a locum tenens physician.
My areas of interest include image processing and computer-vision applications in forensic pathology, policy effects of litigation on practice, inference and diagnostic reasoning, and patterned injury of the skin. I was a member of the FBI Scientific Working Group on Imaging Technologies developing guidelines for forensic imaging, the NIST Organization of Scientific Area Committees – Medicolegal Death Investigation Subcommittee (OSAC-MDI) developing federal standards for death investigation, and am an emeritus member of the Executive Committee of the Applied Image Pattern Recognition Workshop held annually at the Cosmos Club in Washington DC. Prior to retirement, I was on the Board of Directors of the National Association of Medical Examiners.
I have been published in a number of journals and am or have been on the Editorial Boards of Academic Forensic Pathology, Forensic Science, Medicine and Pathology, and the American Journal of Forensic Medicine and Pathology. I have reviewed manuscripts for a number of journals, and have been on numerous grant review committees for the federal government. I have co-authored position papers/white papers for the Centers for Disease Control and Prevention and the Department of Justice.
I am board certified in Anatomic, Clinical, and Forensic Pathology. I am licensed to practice medicine in Tennessee, North Carolina, Georgia, and Virginia.
2. Materials received.
Some folk go into agonizing detail, e.g. exactly how many photographs there are, etc. I don’t do that because I’m not very good at keeping track of those kinds of numbers. So… I mostly just list the files I have on the case. For instance:
Materials Received:
-
A PDF document labeled “Defendant Name Case File” containing:
-
Indictment
-
Investigation report by Det XXX, 12/1/2001
-
Narrative by Witness XXXX, 12/23/2001
-
Statement by Defendant Name 1/15/2002
-
Statement by Friend of Defendant 1/20/2002
-
-
Medical records of Dead Person
- Autopsy report of Dead Person
-
Hospital photographs of Dead Person
-
Deposition of Hospital Doctor, 6/27/2002
-
Deposition of Autopsy Pathologist 7/1/2002
-
Video of a police interview of a young girl (name not given)
-
Photographs of Defendant
-
Deposition of Associated Person 1
-
Deposition of Associated Person 2
-
Photographs of text messages
-
Recorded interview of Defendant
-
Recorded interview of Witness
-
Scene photographs
-
File containing police reports
Obviously, there would be real names instead of “Dead Person,” etc. That’s detail enough for most folk. If opposing counsel has questions, they’ll get back to my counsel and I’ll respond.
3. Mandate:
The mandate section is usually a little idiosyncratic to me. I don’t like to do stream of consciousness reports from which counsel will try to pick out things they find useful. When I take a case, I usually ask counsel to give me specific questions they want answered. That way I know what to focus on. If there’s something in the medical records that they didn’t ask about but should have, I’ll let them know. I’ll often edit the questions a bit so that they make more sense than maybe they did when counsel asked — sometimes counsel doesn’t know exactly what they need to ask and I’ll try to help.
Mandate:
I am asked to respond to the following concerns:
1) What was the cause of death?
2) What is the implication of the “snoring” noted by observers?
3) Was the recovery position appropriately performed?
4) Was there positional asphyxia?
5) Are there implications to the time it took to render aid?
4. Executive Summary:
The executive summary is the shortest possible response to the questions in the mandate. If I want to make some big point, I’ll do it in the summary at the end.
- The cause of death was opiate intoxication
- The snoring observed by the observers was agonal respiration and is not specific to cause of death
- The recovery position was appropriately performed.
- Positional asphyxia is not a concern in this case
- The decedent may have survived had naloxone been applied shortly after collapse. However, this cannot be stated with certainty.
5. Discussion:
In the discussion, I address each of the questions of the mandate at length. I’ll spend a fair amount of time on this part. Again, this is from a different report…
1. The injuries to this young man are consistent with immersion-type scalding burn injuries.
The injuries to Mr. Person are consistent with immersion burn injuries. As one review notes while discussing a case similar to this case (1):
Scald burns are a type of thermal burn involving hot liquid or hot steam. There are generally two different patterns of injury seen with scald burns: splash/spill or flow pattern, and immersion pattern. A single burn event can have separate patterns or combinations of both. In general, splash/spill patterns are produced by the flow of hot liquid as it travels down or over a certain plane of the body. The point of deepest burn is often the area of initial contact; the burn depth lessens as the hot water flows and the liquid cools. Irregular edges and possibly even discrete areas of splash would indicate splashing water as the child is trying move or flail around in response to the heat of the liquid. There may not be significant splash if the child is in a situation where he or she cannot move away or move around much. Immersion pattern burns, on the other hand, are often more uniform in depth and result from that part of the body being submerged or immersed in standing water. Neither of these patterns are pathognomonic of abusive injury; however, splash/spill pattern burns are highly correlated with an accidental manner of injury and immersion pattern burns are highly correlated with an abusive manner of injury.
In cases of scalding burns such as this, the areas of burning and sparing provide a mechanism of estimating the position of the child. Areas where the skin is folded and surfaces are close together provide protection from the hot fluid or steam. In this case, there is scalding of the buttocks, lower back, and groin, with lesser injury to the anterior abdomen. This is consistent with leaning backwards with the buttocks deep in the water, a lesser exposure to the abdomen, with the feet and upper chest out of the water.
Other sources of injury can create similar-appearing injuries, but are largely confined to industrial or laboratory environments, e.g. steam, certain corrosives, etc. These are unlikely in this case.
2. The injuries are near-instantaneous
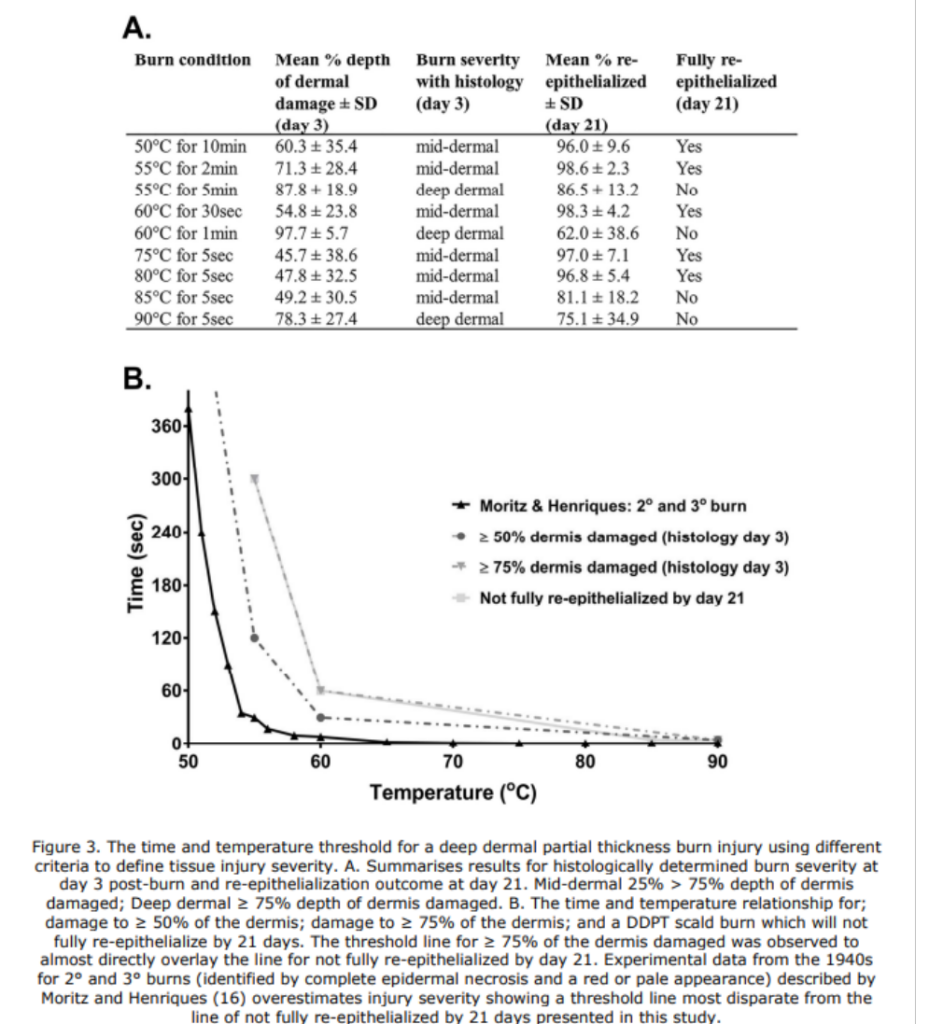
According to the history provided, the water heater was set at 150 degrees F, though during Mr. Johnston’s interview the investigating officer suggested the water was in the mid- to high- 130s. At 150 degrees, deep burns are almost instantaneous. Interestingly, the data seen on most web pages and textbooks derives from early studies done in the late 1940s (2,3,4). Later studies provide a slightly slower burn rate (4). Regardless, at 150 degrees F (65.5 degrees C) severe burns occur in one to a few seconds. At 137 degrees F (58.3 degrees C) severe burns occur in a few seconds. One later study provides a graphic comparison between it’s findings (grey lines) and early studies (black line) (5):
In addition, a conventional hypothesis is that children burn approximately twice as fast as the adults who formed the basis of the 1947 studies (6). Regardless of which study one uses, these injuries could easily be created within a few moments of inattention and do not represent evidence that the child was placed in hot water for an extended period of time.
3. The anatomic features of this injury cannot distinguish between accidental and inflicted injury
3.1 Immersion burns such as these can be accidental.
Immersion burns are more often inflicted than are splash-type wounds. However, splash wounds are often inflicted and immersion injuries are often accidental.
In one study of immersion injuries from bathing infants in a sink, the authors note (6):
There were striking historical similarities in these cases. All involved young toddlers known to play in or around bathroom sinks. The toddlers all had easy climbing access and were left unsupervised for short periods of time. In all of the cases, the parents had previously allowed or encouraged activities near the sink. In addition, the water heaters in all of the homes were set at or above 140°F.
It is clear that children can sustain significant accidental burn injury in sinks, primarily as a result of high water temperatures. The length of time required to produce injuries decreases exponentially as the temperature of water increases. Data exist regarding time to cutaneous burning as a product of the temperature of water in adults.16 It has been hypothesized that at temperatures ⬎130°F, children can burn in one fourth to one half the time of adults. Second and third-degree burns are estimated to occur in 1 second at 140°F and in only half of a second at 149°F.
In one study of bath-related scalding injuries, of 68 injured children only 4 suffered inflicted injury, though it should be noted that this included multiple patterns of scalding, including splash-type scalding (7). Of 226 children admitted to hospitals in New York, 122 were admitted for bathing-related tap water scalds (8). Another study suggests that the likelihood of accidental immersion burns is in part a function of motor development (9).
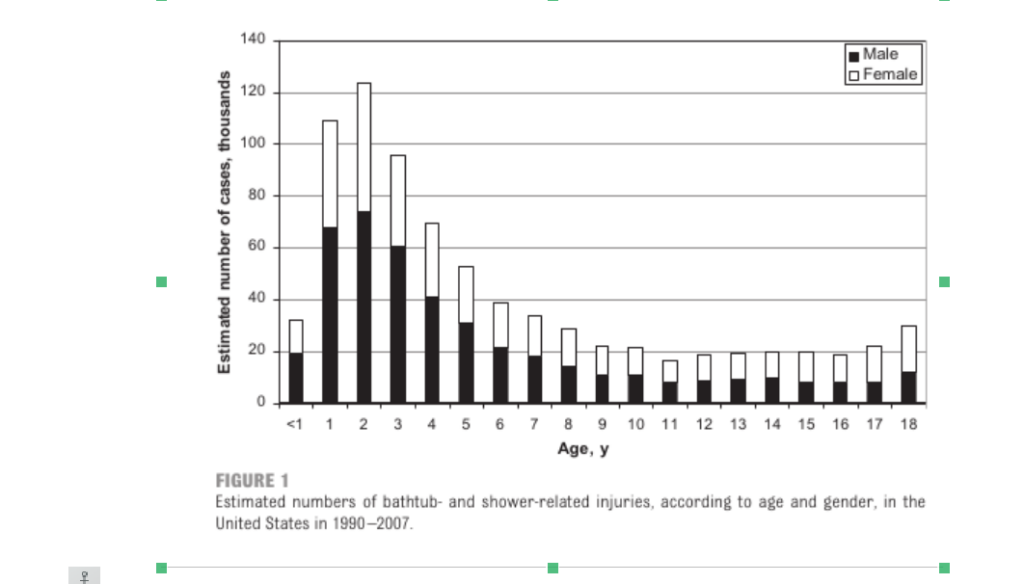
Accidental scalding in the bathtub is not uncommon. One epidemiological study, there were 791,000 accidental bathtub and shower-related injuries among children in the United States. Of these, approximately 30,293 were burn injuries. The distribution of children’s ages in these injuries peaks at the age of 2 years, the same age as the child in this case (10):
The authors note:
As expected, bathtub- and shower-related burns and submersions had much higher rates of hospital admission than did slips, trips, and falls. Several measures are now in effect to help prevent scalding and drowning. As the effects of temperature and duration of exposure to hot water on scald burns became better understood, legislation and educational efforts worked together to decrease preset temperatures on water heaters, which reduced the incidence of hot-water scalds.
3.2 Adequate determination of the likelihood that this was an accidental or inflicted injury requires engineering expertise.
etc…
My technique for this that’s a little different than some others is that I use extended quotes from articles and if at all possible, I provide a reference for every statement about the subject. The reason for this is that a) it makes depositions a lot easier because I know exactly where I got stuff, and b) I’m providing a specific scientific basis for my opinion. Generally, unless it’s an obviously experiential statement (e.g. “In my 35 years of practicing Forensic Pathology, I’ve never seen a person die of reading Hemmingway.”), I will always try to provide a reference.
It also avoids personal attacks from opposing counsel. I really hate it when opposing experts go “There’s no scientific basis for this. Only an incompetent or unethical pathologist would say something like this. This is absurd and represents a lack of integrity.” I’ve seen this a couple of times and it’s really uncalled for. The example I go to more recently is the lynching of Dave Fowler in the George Floyd case, but I’ve seen it a number of times. I’ve had an opposing expert claim that my opinion was based solely in my hatred of the poor, and another (counsel, not expert) because I’m a white male and thus care nothing about the rape of women. If the opposing expert or counsel is one of these assholes, this puts them in the position of having to deal with the literature and not just attacking you as a person.
Finally, providing references for your statements means that you know that your statements are rarely to certainty. All of us learn heuristics in Fellowship and early practice, and there’s a tendency to believe they are writ in stone. They rarely are. I’ve seen a lot of experts get into trouble by being dogmatic about their certainty when in fact the literature does not support that certainty at all. Think time of death determination…
6. Summary:
This section basically a recap of the executive summary. The difference is usually there’s some point I want to emphasize, and this allows me to do that, e.g.
“The death in this case is from multiple blunt trauma. The pattern of injuries are consistent with multiple beatings over an extended period of time. The contention of the opposing expert that these are accidental and from one event are not consistent with the patterned injuries, the placement of injuries, or the varying age of healing. This man was beaten to death.”
7. References:
You know how to do these, so I won’t cut and paste. One thing about references is that you really need to have read them. Don’t get into the habit of just reading abstracts. Get copies of the articles, and save them. Opposing counsel may well ask for them, thinking you are bullshitting them. Never bluff and never lie. One of the great things about doing these consults is that you get to spend time doing literature reviews and get paid for it. It would be better if you got CME for it, but for me it’s fun, and with modern tools for finding and retrieving articles, it’s a great thing to do. Every consult becomes an opportunity to brush up on the latest in the literature, and explore hidden gems in the old literature.
So, that’s how I write a consultation report. I hope you find this useful.