A 70-year-old man was found dead in his apartment. At autopsy, external exam revealed minor trauma consistent with collapse and fall. Internal examination demonstrated emphysema, mild interstitial pneumonia, and alveoli filled with macrophages and occasional giant cells, without granuloma formation. He also had severe coronary artery disease, cardiomegaly, and severe arteriosclerosis of the aorta.
The findings in the lungs were not something that I had run into before. Lungs with giant cells are not that uncommon in today’s world where drug use is common, but these are primarily found in alveolar walls and often form microgranulomata or fully formed granulomata. I’m not used to seeing just the occasional giant cell floating around in alveoli. At the top of the differential is so-called “hard metal lung disease,” which is an interstitial pneumonitis chracterised by macrophages filling up alveoli along with occasional giant cells. Granulomata have been noted, but are rare. There’s often a restrictive lung disease component, with interstitial fibrosis. Bronchiolitis is also common. Hard metal lung disease is seen in people who work with tungsten steel, foundries, and other metal work. More recent studies have suggested that the primary culprit is cobalt, and it’s an autoimmune disease with variable prognosis. It usually stops progressing, and often regresses, once the offending exposures stop.
I talked to the decedent’s family and asked if he had worked in a foundry or something like that. She told me that he had worked in a metal finishing plant making tools for a few years a couple of decades ago.
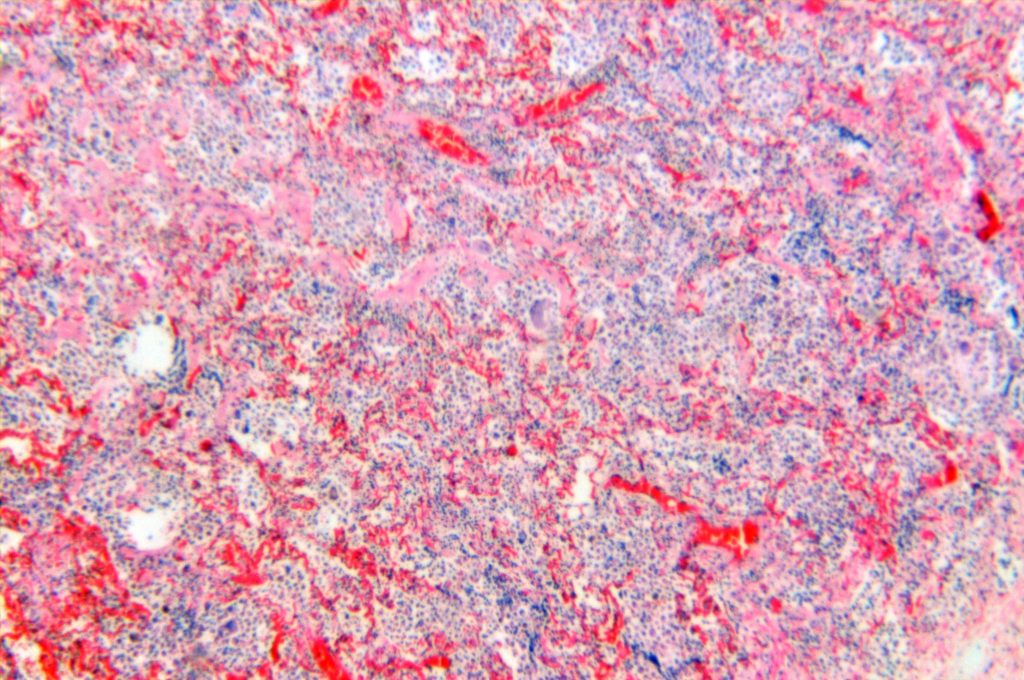
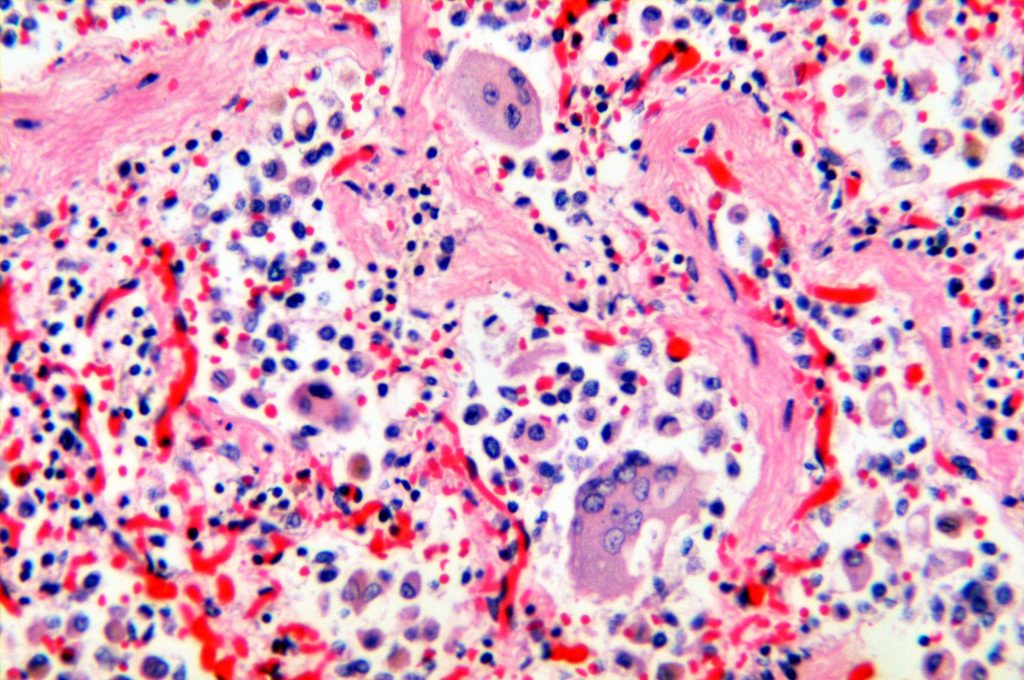
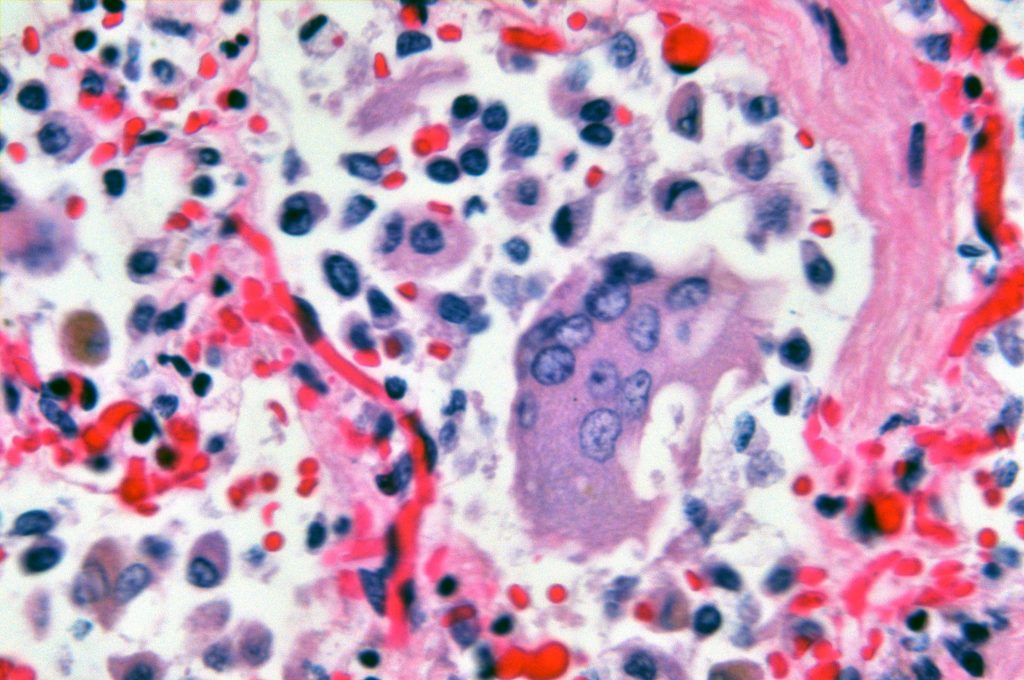
The photographs are not great. This is an earlier case of mine, back when I had a rather poor digital camera and cobbled-together light tubes. Still, it shows some of the primary characteristics.
First, here’s a low power. Yes, it’s fuzzy. Still, you can see the alveoli filled with mononuclear cells and occasional giant cells. There’s expansion and fibrosis of the interstitium in some places. There’s also a bronchiolitis, but it’s hard to make out with poor focus.
Here’s a higher power showing the collection of lymphocytes, macrophages, plasma cells, reactive pneumocytes, and a couple of intraalveolar giant cells, as well as some alveolar wall fibrosis.
Here’s a high power view of one of the giant cells. The giant cells are described as “cannibalistic” in that they are not engulfing foreign material, but enclosing cellular debris.
Because of the severity of the decedent’s heart disease and the suddeness of the death, I classified the cause of death as due to his cardiovascular disease and did not invoke this in this causation. Nonetheless, it makes for an interesting case.
That’s remarkable! How much of the lungs were involved? I don’t see a lot of air passing through that. Did it make it to part 2 at least? Take care, Al
Al Mock
WV Chief
It was patchy. I don’t know how much of the lung was involved, since I only took a couple of sections. I saw it as a cardiac death, not a respiratory one, so I didn’t sample the lungs extensively. I didn’t suspect this until I saw the slides. Yeah, I put it in part 2, since I considered it a stressor.